Prevalence of elevated lipoprotein(a)
- Approximately 1 in 5 people worldwide have elevated Lp(a) levels1
- Lp(a) levels are approximately 70% to ≥90% genetically determined and elevated levels can be passed down in families2
- Lifestyle modifications do not have a significant influence on Lp(a) levels3-5
- Lp(a) levels remain relatively consistent over a lifetime3-5
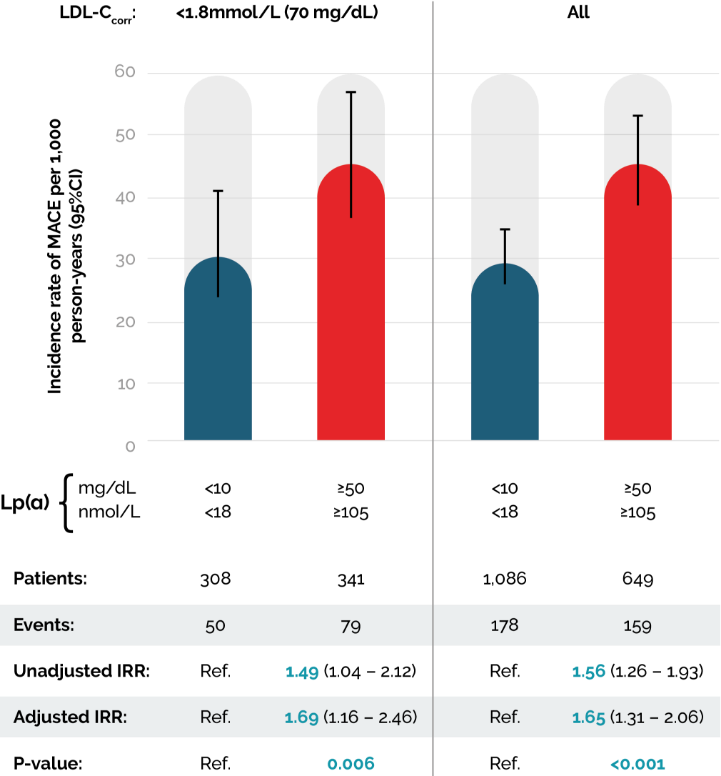
Epidemiological, Mendelian randomisation, and genetic studies involving hundreds of thousands of individuals strongly support a causal and continuous association between Lp(a) level and cardiovascular (CV) outcomes (particularly acute myocardial infarction [MI]) in different ethnicities; even when low-density lipoprotein cholesterol (LDL-C) levels are within the recommended range.4,7-11
A multicentre cross-sectional epidemiological study sought to characterise patterns of Lp(a) levels in a global atherosclerotic cardiovascular disease (ASCVD) population and identify racial, ethnic, regional and gender differences (n=48,135). It was found that Lp(a) is measured in a minority of ASCVD patients (13.9%), and concentrations are highest in Black, young (<65 years), and female patients. More than 25% of patients had levels exceeding the established threshold for increased CV risk, approximately 50 mg/dL or 125 nmol/L.6
Ethnic differences in Lp(a) can be partly explained by differences in LPA gene locus size and single nucleotide polymorphisms. Elevated Lp(a) levels are associated with CV disease risk in all ethnic groups.16
In patients with cardiovascular disease (CVD), elevated Lp(a) independently increases recurrent MACE (Major Adverse Cardiovascular Events)15

Testing for Lp(a)
Building nationwide awareness of the consequences of elevated Lp(a) levels could help to improve the understanding of individual CVD risk. Improved awareness can enhance understanding of population ASCVD risk factors and associated interventions, as well as the CVD risk of family members due to the genetic link. It can also help to inform primary prevention interventions and patient management.
HEART UK and its Lp(a) consensus statement
HEART UK – The UK’s only cholesterol charity
Reducing Lp(a)-associated CV risk requires a reappraisal because:5
- Genetic studies have demonstrated an unequivocal strong link between genes associated with increased Lp(a) and CV risk. Studies have also shown the protective effect of LPA-null alleles or other Lp(a)-decreasing alleles on CVD risk;
- Insights into Lp(a) assay methodology suggest that inaccurate quantitation of Lp(a) has led historically to its underestimation as a cardiovascular risk factor;
- Lp(a) contributes to aortic valve calcification.


The NHS Long Term Plan:
an ongoing solution
Improving ASCVD outcomes is one of the key ambitions within the NHS Long Term Plan as CVD remains the biggest cause of premature mortality. Early detection and treatment of CVD may help extend patient lifespan and improve health.12
Integrated care systems have been instructed to develop joint delivery plans with NHS England to tackle the biggest preventable diseases, starting with CVD.13
Lp(a) Taskforce14
The Lp(a) Taskforce is a diverse multi-stakeholder group that has been constituted to recognise Lp(a) as a key risk factor for ASCVD. Their goal is to raise awareness of the value of screening for Lp(a) in routine clinical practice to improve ASCVD management.
Chaired by HEART UK, the Lp(a) Taskforce comprises members from across the lipid and cardiovascular disease community in the UK. This includes representation from the Association of Clinical Biochemistry and Laboratory Medicine, British Cardiovascular Society, British Atherosclerosis Society, Royal College of Pathologists, Royal Society of Medicine, UK National External Quality Assessment Service, Wales External Quality Assurance Scheme, Novartis Pharmaceuticals, Amgen, Roche Diagnostics and Randox Biosciences.
The Taskforce is calling for the inclusion of Lp(a) in the next update to the National Institute for Health and Care Excellence (NICE) clinical guideline, ‘Cardiovascular disease: risk assessment and reduction, including lipid modification’ (NG238).

References:
- Enas EA, et al. Indian Heart J. 2019 Mar-Apr;71(2):99-112.
- Reyes-Soffer et al. Arteriosclerosis, Thrombosis, and Vascular Biology. 2022;42:e48–e60.
- Enkhmaa B, et al. Nutrients. 2020;12(7):2024.
- Kronenberg F, et al. Eur Heart J. 2022 Oct 14;43(39):3925-3946.
- Cegla J, et al. Atherosclerosis. 2019. 291:62-70
- Nissen SE, et al. Open Heart. 2022 Oct;9(2):e002060.
- Tsimikas S. J Am Coll Cardiol. 2017;69:692-711;
- Erqou S et al. JAMA. 2009;302(4):412-23;
- Kamstrup PR et al. JAMA. 2009;301(22):2331-9;
- Clarke R et al. N Engl J Med. 2009 ;361(26):2518-28;
- Vinci P, et al. Int J Environ Res Public Health. 2023 Sep 6;20(18):6721.
- NHS England. NHSLong-TermPlan.January2019. Available at https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf [Last accessed July 2025]
- Department of Health and Social Care. Health and Social Care Secretary speech on Health Reform. March 2022. Available at https://www.gov.uk/government/speeches/health-and-social-care-secretary-speech-on-health-reform [Last accessed July 2025]
- Lp(a) Taskforce. A call to action from the Lipoprotein(a) Taskforce. Available from: https://www.heartuk.org.uk/downloads/health-professionals/a-call-to-action-from-the-lipoprotein(a)-taskforce---august-2023.pdf [Last accessed July 2025]
- Madsen CM, et al. Arterioscler Thromb Vasc Biol. 2020;40(1):255–266
- Mehta A, et al. Atherosclerosis. 2022 May:349:42-52.
UK | July 2025 | FA-11414802

